COVID-19 Research: With or Without Animals?
Date: Friday, October 16, 2020
Enormous efforts from scientists around the world are furthering our understanding of SARS-CoV-2 infection, in order to develop new, or identify existing, treatments. In the second session, we will use SARS-CoV-2 as an example to discuss why using research methods and tools that are based on human biology is crucial to finding effective and safe treatments and cures for human illnesses.
Key questions include: Which non-human animals are currently used to find treatments for SARS-CoV-2? Why are such procedures done even though it is increasingly evident that results from animal experiments are not predictive of human responses? What innovative non-animal methods are available and now used to tackle the COVID crisis? And why are we still relying on animals for safety testing?
We have seen that some companies may restrain from extensive animal testing in the early phases of vaccine development to accelerate the move to clinical trials. However, does this merely delay the use of animals since later on in the process animals are still used for testing, as this remains a legal requirement? The need for a more agile regulatory processes, and what is required to create regulatory changes that remove animals from these requirements, will also be discussed.
Moderator: Kathrin Herrmann (Johns Hopkins Center for Alternatives to Animal Testing)
Speakers: Aysha Akhtar (Center for Contemporary Sciences), Elizabeth Baker (Physicians Committee for Responsible Medicine), Thomas Hartung (Johns Hopkins Center for Alternatives to Animal Testing), Lindsay Marshall (The Humane Society of the United States/ Humane Society International)
Abstracts
Aysha Akhtar
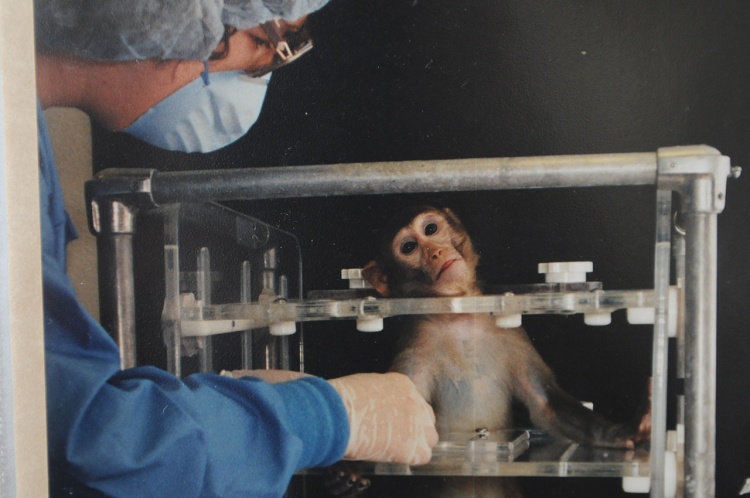
Animal research and testing is defended by arguments that it is reliable, that animals provide sufficiently good models of human biology and diseases, and that consequently its use provides major human health benefits. In this talk, we will demonstrate that a growing body of scientific literature raises important concerns about their reliability and predictive value for human outcomes and for understanding human physiology. The unreliability of animal experimentation across a wide range of areas, including vaccine research, undermines scientific arguments in favor of the practice.
Animal experimentation often significantly harms humans through misleading safety studies, potential abandonment of effective therapeutics, and directing resources away from more effective testing methods. New testing methods that are based on human biology offer the best pathway to study human biology and the diseases that afflict us. The Center for Contemporary Sciences will advance a paradigm shift in the biomedical sciences away from misleading animal experimentation and toward more effective human-specific approaches.
Elizabeth Baker
You have likely heard that animal testing is not predictive of human outcomes. You may also know that newer test methods have been developed that are based on human biology. So why do scientists continue to use animals when human health is at stake, especially during a pandemic? There are many factors at play – and using the best scientific approaches does not top the list.
In this talk, we will examine why animal testing continues to hold center stage in the development of new pharmaceutical treatments, focusing on policies that must be changed because they mandate or prioritize animal experiments. We’ll also discuss FDA policy for fast tracking COVID therapeutics that has allowed companies to move to clinical trials in humans without the usual package of extensive animal studies. Focusing on science alone will not be enough to move past animal testing. Policies that support the use of human biology-based nonclinical approaches are needed to help bring safer and more effective medicines to patients more quickly.
Thomas Hartung
COVID-19 – a game-changer for alternative methods? The unprecedented challenge of COVID-19 opens the door for the application of new approach methods. The virus as a human pathogen shows the need for human models. Species differences in disease, immune response and organ involvement, as well as duration and costs of broad substance testing, are not adequate for the fast response needed to move agents into clinical testing. This is even more so for the broad diversity of biological agents such as human proteins and antibodies evaluated as treatment options.
Advanced cell culture (microphysiological systems) and big data / artificial intelligence have changed the repertoire of alternative methods and lend themselves now to helping to accelerate drug and vaccine development with faster and more human-relevant data. Examples from our own research on SARS-CoV-2 in BrainSpheres and A.I. to predict compound properties are given to illustrate this. So, if it works for COVID-19 why should it not be leveraged for the future? The pandemic may become the dam breach for the broader use of new approaches.
Lindsay Marshall
Human-relevant airways models for disease research: You might think that breathing is the same for all air-breathing animals, and to some extent you would be correct. But just as humans are not gigantic mice, then mice are not merely tiny people, and there are significant differences between the airways of different species. For example, mice and other rodents are obligate nose breathers, and mouse airways have a very different branching pattern and cellular composition compared to humans. Mice are not naturally susceptible to the same infections as people, and this is very relevant today, considering the SARS-CoV2 pandemic.
In this talk, we will consider how the innovative, human cell-based models that can mimic the structure and functions of the human airways, including the lung-on-a-chip, can be exploited to understand, and ultimately defeat, SARS-CoV2. In 2015, the Wyss Institute’s lung-on-a-chip formed part of their human organs-on-chips model awarded the Design of the Year Award by London’s Design Museum. We will take a closer look at this award-winning creation to understand how this, and similar human cell-based models, are being used to decipher how SARS-CoV2 infects us. Application of these human-based models are vital if we are to fully comprehend the human response to the virus and to identify effective treatments. We have known for some time that animals are not accurate predictors of human responses, and the same is true with SARS-CoV2 – infected non-human animals display different symptoms to humans and many animals are not susceptible to this infection. We will see how using human-relevant methods offer a more cost- and time-effective route to revealing the virus’ weak spots in order to discover treatments and to allow us to overcome this devastating pandemic.
Resources
Websites:
Animal-Free Safety Assessment Collaboration
The European Union Reference Laboratory for alternatives to animal testing
Wyss Institute for Biologically Inspired Engineering at Harvard University
National Center for Advancing Translational Sciences
Center for Alternatives to Animal Testing
Physician’s Committee for Responsible Medicine: Early-Career Researchers Advancing 21st Century Science
PCRM/CAAT 2020 Summer School for Innovative Approaches in Science Portal
The NAT database (Non-Animal Technologies) contains information on modern non-animal technologies from various areas of biomedicine and life sciences, based on scientific studies and publications.
Relevant publications (incl. links to full text):
Akhtar, A., 2015. The flaws and human harms of animal experimentation. Cambridge Quarterly of Healthcare Ethics, 24(4), pp.407-419.
Asif, D. and Irshad, M., 2017. Efficacy trials and progress of HIV vaccines. Journal of Cell Science and Therapy, 8, p.265.
Bailey, J. and Balls, M. (2020). Clinical impact of high-profile animal-based research reported in the UK national press. BMJ Open Science 2020;4:e100039. doi: 10.1136/bmjos-2019-100039
Bailey, J., 2018. Does the stress of laboratory life and experimentation on animals adversely affect research data? A critical review. Alternatives to Laboratory Animals, 46(5), pp.291-305.
Barkauskas, C.E., Chung, M.I., Fioret, B., Gao, X., Katsura, H. and Hogan, B.L., 2017. Lung organoids: current uses and future promise. Development, 144(6), pp.986-997.
Benam, K.H., Dauth, S., Hassell, B., Herland, A., Jain, A., Jang, K.J., Karalis, K., Kim, H.J., MacQueen, L., Mahmoodian, R. and Musah, S., 2015. Engineered in vitro disease models. Annual Review of Pathology: Mechanisms of Disease, 10, pp.195-262.
Benam, K.H., Villenave, R., Lucchesi, C., Varone, A., Hubeau, C., Lee, H.H., Alves, S.E., Salmon, M., Ferrante, T.C., Weaver, J.C. and Bahinski, A., 2016. Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nature methods, 13(2), pp.151-157.
Busquet, F., Hartung, T., Pallocca, G., Rovida, C. and Leist, M., 2020. Harnessing the power of novel animal-free test methods for the development of COVID-19 drugs and vaccines. Archives of toxicology, pp.1-10.
Caly, L., Druce, J.D., Catton, M.G., Jans, D.A. and Wagstaff, K.M., 2020. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral research, p.104787.
Chen, X. and Wang, K., 2016. The fate of medications evaluated for ischemic stroke pharmacotherapy over the period 1995–2015. Acta Pharmaceutica Sinica B, 6(6), pp.522-530.
Castelli, V., Cimini, A. and Ferri, C., 2020. Cytokine Storm in COVID-19: “When You Come Out of the Storm, You Won’t Be the Same Person Who Walked in”. Frontiers in Immunology, 11.
Herrmann, K. and Jayne, K., (eds.) 2019. Animal experimentation: Working towards a paradigm change (p. 752). Brill.
Huh, D., Leslie, D.C., Matthews, B.D., Fraser, J.P., Jurek, S., Hamilton, G.A., Thorneloe, K.S., McAlexander, M.A. and Ingber, D.E., 2012. A human disease model of drug toxicity–induced pulmonary edema in a lung-on-a-chip microdevice. Science translational medicine, 4(159), pp.159ra147-159ra147.
Hynes, J., Marshall, L., Adcock, I., Novotny, T., Nic, M., Dibusz, K. and Gribaldo, L., Advanced Non- animal Models in Biomedical Research: Respiratory Tract Diseases, EUR 30334 EN, Publications Office of the European Union, Luxembourg, 2020, ISBN 978-92-76-21380-2, doi:10.2760/725821, JRC118161.
Ingber, D.E., 2020. Is it Time for Reviewer 3 to Request Human Organ Chip Experiments Instead of Animal Validation Studies?. Advanced Science, p.2002030.
Kozorovitskiy, Y., Gross, C.G., Kopil, C., Battaglia, L., McBreen, M., Stranahan, A.M. and Gould, E., 2005. Experience induces structural and biochemical changes in the adult primate brain. Proceedings of the National Academy of Sciences, 102(48), pp.17478-17482.
Lukassen, S., Chua, R.L., Trefzer, T., Kahn, N.C., Schneider, M.A., Muley, T., Winter, H., Meister, M., Veith, C., Boots, A.W. and Hennig, B.P., 2020. SARS‐CoV‐2 receptor ACE 2 and TMPRSS 2 are primarily expressed in bronchial transient secretory cells. The EMBO journal, 39(10), p.e105114.
Monteil, V., Kwon, H., Prado, P., Hagelkrüys, A., Wimmer, R.A., Stahl, M., Leopoldi, A., Garreta, E., Del Pozo, C.H., Prosper, F. and Romero, J.P., 2020. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell.
Pound, P. and Ritskes-Hoitinga, M., 2018. Is it possible to overcome issues of external validity in preclinical animal research? Why most animal models are bound to fail. Journal of Translational Medicine, 16(1), pp.1-8.
Singh, T.U., Parida, S., Lingaraju, M.C., Kesavan, M., Kumar, D. and Singh, R.K., 2020. Drug repurposing approach to fight COVID-19. Pharmacological Reports, pp.1-30.
Sung, N.S., Crowley Jr, W.F., Genel, M., Salber, P., Sandy, L., Sherwood, L.M., Johnson, S.B., Catanese, V., Tilson, H., Getz, K. and Larson, E.L., 2003. Central challenges facing the national clinical research enterprise. Jama, 289(10), pp.1278-1287.
van der Naald, M., Wenker, S., Doevendans, P.A., Wever, K.E. and Chamuleau, S.A., 2020. Publication rate in preclinical research: a plea for preregistration. BMJ Open Science, 4(1), p.e100051.
Zimmerling, A. and Chen, X., 2020. Bioprinting for combating infectious diseases. Bioprinting, p.e00104.
Other recent articles:
Asthana, S. (2020). Why Rhesus monkeys are used for most vaccine trials. Interview with Prof. Thomas Hartung. The Times of India
Bailey, J. (2020). Repeating Nonhuman Primate Tests of COVID-19 Vaccines is a Folly: Human Vaccine Development Must Focus on Human Biology. ScienceMag
Chawla, D.S. (2020). Millions of animals may be missing from scientific studies. ScienceMag.
Leng, G. and Leng, R. (2020). Unintended Consequences: The Perils of Publication and Citation Bias. The MIT Press Reader.
Staley, O. (2019). The future of stroke patients may depend on the part-time job of a Canadian surgeon. Quartz
Whitehead, N. (2020). A $100 Million HIV Vaccine Project Failed. But All Hope Is Not Lost. NPR.
World Health Organization on HIV Vaccines